Will Severs Disease Demand Surgical Procedures?
Severs disease, also known as calcaneal apophysitis, is a condition in which the growth plate along the heel becomes inflamed. It most commonly occurs in active, early-teen children. Most patients with Severs disease complain of heel pain. In general the pain is exacerbated with increased activities, such as running, jumping, or climbing stairs. The pain often improves with a period of rest.
Causes
The heel bone sometimes grows faster than the leg muscles (including the calf muscles) and tendons (including the Achilles tendon) during the early puberty growth spurt. The different growth rate in these structures can cause lower leg muscles and tendons to become overstretched and tight, which makes the heel less flexible and puts excessive pressure on the heel growth plate. The Achilles tendon, the strongest tendon in the body, attaches to the heel growth plate, and repetitive stress on this structure, especially if it?s already tight, can damage the growth plate, leading to tenderness, swelling, and pain. Activities that involve running or jumping, such as soccer, gymnastics, track, and basketball, can place significant stress on a tight Achilles tendon and contribute to the onset of Sever?s disease. Ill-fitting shoes can also contribute to this health problem by failing to provide the right kind of support or by rubbing against the back of heel. The following factors may increase the likelihood of Sever?s disease in kids or young teens. Wearing footwear that is too narrow in the toe box. Leg length inequality. Obesity or carrying excess bodyweight. Excessive foot and ankle pronation.
Symptoms
Pain symptoms usually begin after a child begins a new sport or sporting season, and can worsen with athletic activities that involve running and jumping. It is common for a child with Sever?s disease to walk with a limp. Increased activity can lead to heel cord tightness (Achilles Tendon), resulting in pressure on the apophysis of the calcaneus. This will cause irritation of the growth plate and sometimes swelling in the heel area thus producing pain. This usually occurs in the early stages of puberty.
Diagnosis
A physical exam of the heel will show tenderness over the back of the heel but not in the Achilles tendon or plantar fascia. There may be tightness in the calf muscle, which contributes to tension on the heel. The tendons in the heel get stretched more in patients with flat feet. There is greater impact force on the heels of athletes with a high-arched, rigid foot. The doctor may order an x-ray because x-rays can confirm how mature the growth center is and if there are other sources of heel pain, such as a stress fracture or bone cyst. However, x-rays are not necessary to diagnose Sever?s disease, and it is not possible to make the diagnosis based on the x-ray alone.
Non Surgical Treatment
The doctor might recommend that a child with Sever's disease. perform foot and leg exercises to stretch and strengthen the leg muscles and tendons, elevate and apply ice (wrapped in a towel, not applied directly to the skin) to the injured heel for 20 minutes two or three times per day, even on days when the pain is not that bad, to help reduce swelling, use an elastic wrap or compression stocking that is designed to help decrease pain and swelling, take an over-the-counter medicine to reduce pain and swelling, such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin).
Exercise
Stretching exercises can help. It is important that your child performs exercises to stretch the hamstring and calf muscles, and the tendons on the back of the leg. The child should do these stretches 2 or 3 times a day. Each stretch should be held for about 20 seconds. Both legs should be stretched, even if the pain is only in 1 heel. Your child also needs to do exercises to strengthen the muscles on the front of the shin. To do this, your child should sit on the floor, keeping his or her hurt leg straight. One end of a bungee cord or piece of rubber tubing is hooked around a table leg. The other end is hitched around the child's toes. The child then scoots back just far enough to stretch the cord. Next, the child slowly bends the foot toward his or her body. When the child cannot bend the foot any closer, he or she slowly points the foot in the opposite direction (toward the table). This exercise (15 repetitions of "foot curling") should be done about 3 times. The child should do this exercise routine a few times daily.
Causes And Treatments
Overview
Just as an old bridge would become unsafe as the structure was compromised, your feet can experience the same. If you have PTTD and the tendon continues to weaken, it simply won?t be able hold up your arch. In this situation, the arch can fall or collapse, which is referred to as adult-acquired flat foot. You may experience pain and tenderness behind the inside of the ankle. Over time, in addition to the flattening of the foot, you may also notice a misalignment of the heel so that it no longer aligns underneath the rest of the leg. A tightening of the heel cord, arthritis, and possible deformity of the ankle joint may also occur. You may feel the discomfort move from the inside to the outside of the ankle as well. Flat foot can also contribute to problems with the plantar fascia, which is the tendon that runs along the length of your arch. 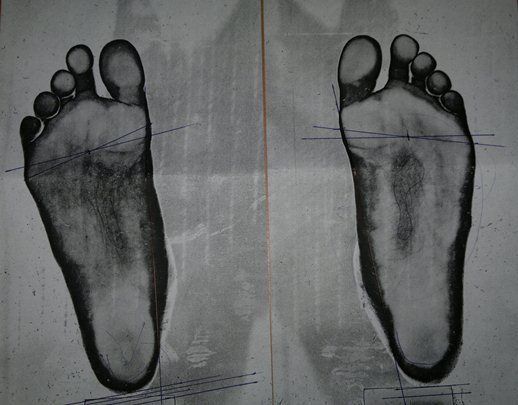
Causes
As the name suggests, adult-acquired flatfoot occurs once musculoskeletal maturity is reached, and it can present for a number of reasons, though one stands out among the others. While fractures, dislocations, tendon lacerations, and other such traumatic events do contribute to adult-acquired flatfoot as a significant lower extremity disorder, as mentioned above, damage to the posterior tibial tendon is most often at the heart of adult-acquired flatfoot. One study further elaborates on the matter by concluding that ?60% of patients [presenting with posterior tibial tendon damage and adult-acquired flatfoot] were obese or had diabetes mellitus, hypertension, previous surgery or trauma to the medial foot, or treatment with steroids?.
Symptoms
PTTD begins with a gradual stretching and loss of strength of the posterior tibial tendon which is the most important tendon supporting the arch of the human foot. Left untreated, this tendon will continue to lengthen and eventually rupture, leading to a progressive visible collapse of the arch of the foot. In the early stages, patients with PTTD will notice a pain and swelling along the inner ankle and arch. Many times, they are diagnosed with ?tendonitis? of the inner ankle. If the foot and ankle are not properly supported during this early phase, the posterior tibial tendon can rupture and devastating consequences will occur to the foot and ankle structure. The progressive adult acquired flatfoot deformity will cause the heel to roll inward in a ?valgus? or pronated direction while the forefoot will rotate outward causing a ?duckfooted? walking pattern. Eventually, significant arthritis can occur in the joints of the foot, the ankle and even the knee. Early diagnosis and treatment is critical so if you have noticed that one, or both, of your feet has become flatter in recent times come in and have it checked out.
Diagnosis
Clinicians need to recognize the early stage of this syndrome which includes pain, swelling, tendonitis and disability. The musculoskeletal portion of the clinical exam can help determine the stage of the disease. It is important to palpate the posterior tibial tendon and test its muscle strength. This is tested by asking patient to plantarflex and invert the foot. Joint range of motion is should be assessed as well. Stiffness of the joints may indicate longstanding disease causing a rigid deformity. A weightbearing examination should be performed as well. A complete absence of the medial longitudinal arch is often seen. In later stages the head of the talus bone projects outward to the point of a large "lump" in the arch. Observing the patient's feet from behind shows a significant valgus rotation of the heel. From behind, the "too many toes" sign may be seen as well. This is when there is abducution of the forefoot in the transverse plane allowing the toes to be seen from behind. Dysfunction of the posterior tibial tendon can be assessed by asking the patient to stand on his/her toes on the affected foot. If they are unable to, this indicates the disease is in a more advanced stage with the tendon possibly completely ruptured.
Non surgical Treatment
Nonoperative treatment of posterior tibial tendon dysfunction can be successful with the Arizona AFO brace, particularly when treatment is initiated in the early stages of the disease. This mandates that the orthopedist has a high index of suspicion when evaluating patients to make an accurate diagnosis. Although there is a role for surgical management of acquired flat feet, a well-fitted, custom-molded leather and polypropylene orthosis can be effective at relieving symptoms and either obviating or delaying any surgical intervention. In today's climate of patient satisfaction directed health care, a less invasive treatment modality that relieves pain may prove to be more valuable than similar pain relief that is obtained after surgery. Questions regarding the long-term results of bracing remain unanswered. Future studies are needed to determine if disease progression and arthrosis occur despite symptomatic relief with a brace. Furthermore, age- and disease stage-matched control groups who are randomized to undergo surgery or bracing are necessary to compare these different treatment modalities. 
Surgical Treatment
The indications for surgery are persistent pain and/or significant deformity. Sometimes the foot just feels weak and the assessment of deformity is best done by a foot and ankle specialist. If surgery is appropriate, a combination of soft tissue and bony procedures may be considered to correct alignment and support the medial arch, taking strain off failing ligaments. Depending upon the tissues involved and extent of deformity, the foot and ankle specialist will determine the necessary combination of procedures. Surgical procedures may include a medial slide calcaneal osteotomy to correct position of the heel, a lateral column lengthening to correct position in the midfoot and a medial cuneiform osteotomy or first metatarsal-tarsal fusion to correct elevation of the medial forefoot. The posterior tibial tendon may be reconstructed with a tendon transfer. In severe cases (stage III), the reconstruction may include fusion of the hind foot,, resulting in stiffness of the hind foot but the desired pain relief. In the most severe stage (stage IV), the deltoid ligament on the inside of the ankle fails, resulting in the deformity in the ankle. This deformity over time can result in arthritis in the ankle.
High Arch Pain Exercises
A cavus or high-arched foot may have many foot shapes. This may range from an arch that is slightly high to a severe deformity that causes a patient to walk on the outside of the foot. Surgery is occasionally required to realign the foot. There are different causes of a high-arched foot. In many cases, the cause is unknown. In other cases, the cause is a nerve disease, clubfoot or injury. Treatment ranges from changes in shoewear to surgeries, depending on the amount of deformity and related problems.
Causes
The most common cause of arch pain is plantar fasciitis. Plantar fasciitis is the name that describes inflammation of the fibrous band of tissue that connects the heel to the toes. Symptoms of plantar fasciitis include pain early in the morning and pain with long walks or prolonged standing. Arch pain early in the morning is due to the plantar fascia becoming contracted and tight as you sleep through the night. When awakening and walking in the morning, the fascia is still tight and prone to irritation when stretched. When walking or standing for long periods, the plantar fascia becomes inflamed and painful. Treatment of plantar fasciitis is best accomplished with some simple stretching exercises, anti-inflammatory medications, and inserts for your shoes.
Symptoms
Arch pain may have a variety of different causes. Proper evaluation and diagnosis of arch pain is essential in planning treatment. A good general guideline is to compare the injured side to the uninjured side. Injury may present itself as a distinguishable lump, a gap felt at that location, or a "crunchy" feeling on that spot caused by inflammation. The type, causes, and severity of pain are also good indicators of the severity of the injury.
Diagnosis
The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
Non Surgical Treatment
One of the most successful, and practical treatments recommended by podiatrists are orthotic devices, sometimes referred to as arch supports. Orthotics take various forms and are constructed of various materials, usually best recommended by your doctor to address the severity of your problem. All orthotic devices serve to improve foot function and minimize stress forces that could ultimately arch pain.

Surgical Treatment
Surgery may be necessary in situations where the symptoms are likely to get worse over time, or when pain and instability cannot be corrected with external orthopedic devices. There are many types of surgical procedures, including cavus foot reconstruction, which can be performed to correct the foot and the ankle and restore function and muscle balance.
Prevention
There are several things that you can do to prevent and treat arch pain. This includes Avoiding high heeled shoes, Stretching the calf muscles regularly, Wearing well fitted, comfortable shoes, Using customisedorthotic devices or shoe inserts, Elevating the feet and applying ice and taking over-the-counter anti-inflammatory medications. You can also care for your feet by paying attention to any changes in your feet as you get older. It is normal for feet to lose some of their fat pads as a person ages. Your feet may get bigger, both wider and longer as well. Make sure that you wear shoes that are sturdy, but comfortable, and have your feet measured before you buy shoes to make sure that you are still wearing the right size. Shoe sizes vary from one brand to the next, so it is a good idea to have your feet measured every time you purchase shoes. When choosing shoes, match the shoe to the activity for which it will be worn. Within the broader grouping of athletic shoes, there are different categories with different features. For example, a running shoe has different features than a walking shoe. You may develop some arthritic changes in your feet over time, too. If you notice that you are experiencing more pain in your feet, see your doctor for an evaluation. If the pain is arthritis-related, your doctor may recommend medication or other treatment to slow the progression of the arthritis.
Stretching Exercises
Calf Stretching in Bed. As you may already know, the first few steps out of bed in the morning can be the worst of the day. Those first few steps can be enough to reaggravate your condition putting you into a cycle of inflammation and pain. The best way to help break that cycle is to stretch your calf before taking those first steps in the morning. When the muscles in your calf are tight, they pull on the heel bone, making your plantar fascia very taut and prone to injury. To help loosen those muscles, take a towel or belt and loop it around the ball of your foot. Keeping your leg straight, gently pull towards your body until you feel a stretch in the lower part of your leg. Hold that for 30 seconds and repeat up to 5 times before taking your first step out of bed. Plantar Fascia Stretching. Loosening up the tissues that are irritated probably makes sense to you, but you may not know how to do so. Luckily, there?s a very simple way. All you have to do is pull your toes up with your hand until you feel a stretch along the ball of your foot. You may feel the stretch anywhere from the ball of your foot to your heel. Holding this position for 30 seconds a few times can make a world of difference in your pain levels. Calf Stretching. I know, it probably seems like overkill, but stretching out the muscles in the lower leg is an integral step to recovery. There are two main muscles in the lower leg that attach to the heel, so we?ll work on stretching them both out. Stand against a wall and slide one leg back, pushing the heel down towards the floor (first picture). When you feel a stretch in the lower part of your leg, hold it for 30 seconds. After those 30 seconds are up, bend your knees until a deeper stretch is felt a bit lower in the leg (second photo). Again, hold this stretch for 30 seconds and repeat this until you?ve done it 3 times on each leg. Who doesn?t love a good massage? I suppose you could pay for someone to rub out the tissues in the bottom of your foot, but if you?re looking for a cheaper alternative, look no further than the humble tennis ball. Placing a tennis ball on the ground and gently rolling it under foot for a few minutes can help loosen up your plantar fascia, making it much less likely to become irritated. Put enough pressure on the ball to get a deep massage. You may feel some soreness, but back off if you feel any pain.Tennis Ball Massage While using the tennis ball is great for keeping things loose, sometimes it?s worth doing some icing at the same time for some inflammation control. Freezing a water bottle and rolling it under your foot for 10 minutes at the end of the day can be a very effective way to keep inflammation in check while staying loose. It might not be the most comfortable thing in the world, but ?Brrr? is better than ?Ouch? any day. One thing to keep in mind is that while these tips have been proven to work, they?re not an instant fix. It can take a few weeks of consistency with them before your pain levels begin to change. If you?re not seeing any improvement after making an honest effort, it may be time to look into some different treatment methods with your doctor such as formal PT, orthotics, a weight-loss plan, or others.
What Will Cause Achilles Tendonitis Pains ?
 You?re a prime candidate for acquiring Achilles Tendonitis if you?re a runner or some other kind of athlete requiring heavy use of your calves and their attached tendons. Then again, -anybody- can get tendonitis of the Achilles tendons. All for very predictable reasons. Perhaps you have Achilles Tendon pain from cycling. Or standing at work. Or walking around a lot. Anything we do on our feet uses our lower leg structures, and the Achilles tendon bears LOTS of torque, force, load, etc. The physical dynamic called Tendonitis can show up anywhere. On the Achilles Tendon is as good a place as any. Repetitive strain injury can show up anywhere in the body that there is repetitive strain. It's an obvious statement, but worth paying attention to.
You?re a prime candidate for acquiring Achilles Tendonitis if you?re a runner or some other kind of athlete requiring heavy use of your calves and their attached tendons. Then again, -anybody- can get tendonitis of the Achilles tendons. All for very predictable reasons. Perhaps you have Achilles Tendon pain from cycling. Or standing at work. Or walking around a lot. Anything we do on our feet uses our lower leg structures, and the Achilles tendon bears LOTS of torque, force, load, etc. The physical dynamic called Tendonitis can show up anywhere. On the Achilles Tendon is as good a place as any. Repetitive strain injury can show up anywhere in the body that there is repetitive strain. It's an obvious statement, but worth paying attention to.
Causes
The calf is under a lot of strain when running: it is not only put on stretch during landing of the foot, but it also has to produce the tension needed to support body weight and absorb the shock of landing. This is what is called an ?eccentric load?. Excessive eccentric loading - either by way of a dramatic increase in mileage, or excessive hill running, or faulty running posture - could very well be the cause of a runner?s achilles tendinitis. The calf strain translates downward into the achilles tendon where it attaches to the heel, and inflammation ensues. Inflammation then causes scarring and fibrosis of tissues, which in turn inflicts pain upon stretching or use. Risk factors for Achilles tendinitis also include spending prolonged amounts of time standing or walking.
Symptoms
Symptoms of Achilles tendonitis include, pain in the back of the heel, difficulty walking, sometimes the pain makes walking impossible, swelling, tenderness and warmth of the Achilles tendon. Achilles tendonitis is graded according to how severe it is, mild - pain in the Achilles tendon during a particular activity (such as running) or shortly after. Moderate - the Achilles tendon may swell. In some cases, a hard lump (nodule) may form in the tendon. Severe - any type of activity that involves weight bearing causes pain of the Achilles tendon. Very occasionally, the Achilles tendon may rupture (tear). When an Achilles tendon ruptures, it is said to feel like a hard whack on the heel.
Diagnosis
If Achilles tendonitis is suspected, avoid any exercise or activity that causes the pain. It is advisable to see a doctor promptly so that an accurate diagnosis can be made and appropriate treatment recommended. The doctor will take a full medical history and will ask about the nature and duration of the symptoms. They will perform a physical examination of the affected area. Ultrasound scanning may be used to assess damage to the tendon or surrounding structures. Occasionally MRI (magnetic resonance imaging) may be recommended. The symptoms of Achilles tendonitis are often similar to symptoms of other conditions such as partial Achilles tendon rupture and heel bursitis. This can make diagnosis difficult and a referral to an orthopaedic specialist may be required in order for an accurate diagnosis to be made.
Nonsurgical Treatment
Massage therapy improves blood flow to the muscles and tissues of the affected area while increasing range of motion and can prevent recurring injury. The healing process can be quickened using ultrasound heat therapy to improve blood flow to the affected area. Wearing a night brace keeps the leg flexed, preventing stiffening of the tendon, which would impair healing. Stretching exercises increase flexibility and allow the tendon to heal without shortening, a deformity resulting in chronic pain. Persistent Achilles pain may warrant the use of a cast or walking boot to be worn for 4-6 weeks stabilizing the tendon so it can heal. After removal of the cast or boot, physical therapy will be ordered to increase functionality of the affected limb. To reduce chronic inflammation of the tendon, corticosteroid injections may be prescribed. It?s important to note that this corticosteroid treatment increases the risk of tendon rupture. Ultrasound imaging may be used by the physician administering the steroid injection, in order to help visualize the affected area. When all other therapies have failed to or tendon rupture occurs, surgical intervention and repair of the muscles and tendons is the last treatment option.

Surgical Treatment
Surgery usually isn't needed to treat Achilles tendinopathy. But in rare cases, someone might consider surgery when rubbing between the tendon and the tissue covering the tendon (tendon sheath) causes the sheath to become thick and fibrous. Surgery can be done to remove the fibrous tissue and repair any small tendon tears. This may also help prevent an Achilles tendon rupture.
Prevention
Do strengthening and stretching exercises to keep calf muscles strong and flexible. Keep your hamstring muscles flexible by stretching. Warm up and stretch adequately before participating in any sports. Always increase the intensity and duration of training gradually. Do not continue an exercise if you experience pain over the tendon. Wear properly fitted running and other sports shoes, including properly fitted arch supports if your feet roll inwards excessively (over-pronate).
Are Fallen Arches Flat Feet?

If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics can be prescribed to create a system of support for the body and surgery can also offer a more permanent solution. Contact us today to discuss which treatment option may be right for you.
Causes
Footwear: shoes which limit toe movement; high heels. Barefoot walking may be protective. A tight Achilles tendon or calf muscles (heel cord contracture). This may help to cause Pes Planus, or may contribute to symptoms such as foot pain when there is existing Pes Planus. Obesity. Other bony abnormalities, eg rotational deformities, tibial abnormalities, coalition (fusion) of tarsal bones, equinus deformity. Ligamentous laxity, eg familial, Marfan's syndrome, Ehlers-Danlos syndrome, Down's syndrome. Other factors causing foot pronation, eg hip abductor weakness and genu valgum.
Symptoms
Structural problems in your feet like fallen arches can alter your walking pattern, running pattern and cause pain throughout your body. Clear and accurate assessment of the mechanics of your lower limbs is key to understanding the profound effect that subtle faults in your foot, ankle, knee and hip alignment can cause.
Diagnosis
It is important for people with foot pain to know if they have flat feet. The following tests can help you determine your arch type. When you get out of a swimming pool, look at your footprint on the concrete. The front of the foot will be joined to the heel by a strip. If your foot is flat, then the strip is the same width as the front of the foot, creating a footprint that looks like a stretched out pancake. With a normal arch, the strip is about half the width of the front of the foot. If you have a high arch, only a thin strip connects the front of the foot with the heel. Put your shoes on a flat table and view them at eye level from behind. See if the sole is worn evenly. A flat foot will cause more wear on the inside of the sole, especially in the heel area. The shoe will easily rock side to side. A flat foot will also cause the upper part of the shoe to lean inward over the sole. Both shoes should wear about the same way. If you have pain in one foot, you should make sure you don't have a fallen arch on that side. There are two good tests you can perform at home to detect this problem. Place your fingertips on a wall that you are directly facing and stand on your tiptoes on one foot. If you can't do it, a fallen arch may be the culprit. Stand with your feet parallel. Have someone stand in back of you and look at your feet from behind. You can also do it yourself if you stand with your back to a mirror. Normally, only the pinky toe is visible from behind. If one foot is flatter than the other, the 4th and sometimes the 3rd toe on that foot can also be seen.
Non Surgical Treatment
Physiotherapists will carry out a detailed biomechanical assessment of your feet and lower limb. Once the causes have been identified a number of treatment methods may be used to help relieve pain and restore function in the feet including the use of custom made orthotics to support the foot and offload the areas which are painful, strengthening exercises for weakened muscles and tendons in the arch, and massage and mobilisation techniques to help mobilise stiff tissue and joints in the foot.
Surgical Treatment

Surgical correction is dependent on the severity of symptoms and the stage of deformity. The goals of surgery are to create a more functional and stable foot. There are multiple procedures available to the surgeon and it may take several to correct a flatfoot deformity. Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. Usually surgical treatment begins with removal of inflammatory tissue and repair of the posterior tibial tendon. A tendon transfer is performed if the posterior tibial muscle is weak or the tendon is badly damaged. The most commonly used tendon is the flexor digitorum longus tendon. This tendon flexes or moves the lesser toes downward. The flexor digitorum longus tendon is utilized due to its close proximity to the posterior tibial tendon and because there are minimal side effects with its loss. The remainder of the tendon is sutured to the flexor hallucis longus tendon that flexes the big toe so that little function is loss. Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
How Do Bunions Start

A bunion is a prominence over the inside part of the foot where the big toe joins the rest of the foot. Pressure on the prominence from shoes causes pain and swelling due to inflammation. The bunion occurs when the foot bone connecting to the big toe (the first metatarsal) moves gradually towards the opposite foot. This is called hallux valgus deformity. This leads to the big toe being pushed towards the second toe (away from the opposite foot) so that the big toe points away from the other foot. Other problems can develop with a bunion. For example the second toe may overlap the big toe causing a cross-over toe deformity. With shoe pressure, corns and calluses develop.
Causes
Bunions most commonly affect women. Some studies report that bunions occur nearly 10 times more frequently in women. It has been suggested that tight-fitting shoes, especially high-heel and narrow-toed shoes, might increase the risk for bunion formation. Bunions are reported to be more prevalent in people who wear shoes than in barefoot people. While the precise causes are not known, there also seems to be inherited (genetic) factors that predispose to the development of bunions, especially when they occur in younger individuals. Other risk factors for the development of bunions include abnormal formation of the bones of the foot at birth (congenital), nerve conditions that affect the foot, rheumatoid arthritis, and injury to the foot. Bunions are common in ballet dancers.
Symptoms
Bunions may cause no pain at first. But as the big toe begins to turn in towards the other toes, people with bunions usually experience redness, pain, swelling, and tenderness in the area around the joint. Pressure inside the joint or from footwear pressing against the bunion may also cause discomfort. As the affected toe curves closer to the other toes on the foot, these toes can become painful as well. Complications of bunions include corns, calluses, hammer toe, and ingrown toenails. Other complications include irritation of the nerves surrounding the bunion area. Excess rubbing of the bunion against the footwear may lead to changes in the skin, resulting in corns or calluses. Hammer toe is a deformity of the toe immediately next to the big toe. A hammer toe is slightly raised and points upwards from the base and downwards at the end of the toe. Ingrown toenails can result from increased pressure from the big toe on the other toes. There may also be a decrease in the amount a person can move the joint affected by the bunion. Irritation of the nerves will feel like burning or decreased sensation.
Diagnosis
Before examining your foot, the doctor will ask you about the types of shoes you wear and how often you wear them. He or she also will ask if anyone else in your family has had bunions or if you have had any previous injury to the foot. In most cases, your doctor can diagnose a bunion just by examining your foot. During this exam, you will be asked to move your big toe up and down to see if you can move it as much as you should be able to. The doctor also will look for signs of redness and swelling and ask if the area is painful. Your doctor may want to order X-rays of the foot to check for other causes of pain, to determine whether there is significant arthritis and to see if the bones are aligned properly.
Non Surgical Treatment
Apply a commercial bunion pad around the bony prominence, use only non-medicated pads. Wear shoes with a wide and deep toe box. You should be able to "dimple" the leather over your bunion. Avoid all high heeled shoes. If your bunion becomes painful red, and swollen try elevating your foot and applying ice for about 20 minuets every hour. If symptoms persist, consult your podiatrist or physician.

Surgical Treatment
When the pain of a bunion interferes with daily activities, and conservative treatment has been completed it's time to discuss surgical options. Foot Mechanics has excellent relationships with many Orthopaedic Surgeons, who are the specialists who perform bunion surgery. Because bunions are caused by faulty foot mechanics surgery can improve the look of your feet by removing the ?bump? but if the underlying mechanics are not addressed then the bunion is likely to return. For this reason orthotics are used post-surgery to prevent the return of bunions.
The Causes Of Pain In The Arches ?
Plantar fasciitis refers to an inflammation of the plantar fascia, a thick, fibrous band running along the sole of the foot. Such inflammation results from direct injury to the plantar fascia, usually, repeated trauma to the tissue where the fascia attaches to the calcaneus or heel bone. The plantar fascia is critical in maintaining the foot?s complex arch system, also playing a role in balance and fine control of certain phases of the athlete?s gait. Injury to the plantar fascia is particularly painful and disabling for runners and can often prove stubbornly resistant to treatment. Rehabilitation is frequently a lengthy and frustrating process. For these reasons, care should be taken where possible to avoid such injury by means of preventative exercises and sensitivity to early warning signs.

Causes
Spending a lot of time on your feet. Especially when you are not used to doing so. For example you may have started a new job such as waiting tables where you are on your feet all day and wake up the next day with sore feet. This is a sign of damage and over time could lead to plantar fasciitis. Being Over-Weight. Never an easy topic to discuss but in simple terms, the heavier you are, the greater the burden on your feet. There are times when you're walking when your entire body weight is borne on one leg and therefore one foot, placing great strain on the plantar fascia. Wearing shoes with poor arch support or cushioning. A tight Achilles tendon. This is the big tendon at the bottom of your calf muscles above your heel. If this is excessively tight this can affect your ability to flex your ankle and make you more likely to damage your plantar fascia. Suddenly changing your exercise routine. Using running as an example if you suddenly run many more miles than your are used to or change to a new running surface e.g. grass to tarmac - these factors can put excessive strain on the plantar fascia and lead to plantar fasciitis. All of these risk factors ultimately lead to a specific change in foot structure. The term given is over-pronation and this basically describes rolling in of the foot and lowering of the arches. It is this change that excessively elongates the plantar fascia which can lead to plantar fasciitis.
Symptoms
Plantar fasciitis is most often seen in middle-aged men and women, but can be found in all age groups. The condition is diagnosed with the classic symptoms of pain well focused deep in the heel area of the bottom of the foot. Often the pain from plantar fasciitis is most severe when you first stand on your feet in the morning. Pain often subsides quite quickly, but then returns after prolonged standing or walking. Plantar fasciitis is sometimes, but not always, associated with a rapid gain of weight. It is also sometimes seen in recreational athletes, especially runners. In these athletes, it is thought that the repetitive nature of the sports causes the damage to the fibrous tissue that forms the arch of the foot.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
The initial treatment for arch pain, especially if it is of sudden onset is the use of ice to reduce the swelling. Later heat and anti-inflammatory gels can be a big help. Activity should be modified, if you stand a lot at work, see if you can using seating more, if you run a lot, consider swimming or cycling for a while. Use footwear that is supportive in the midfoot and heel area.

Surgical Treatment
Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Maintain a healthy weight, Use insoles to support your arches, Limit how often you wear high heels, Use proper shoes, especially when exercising to evenly distribute weight through your foot.